
An interview with Sally Watkins, PhD, MS, RN
WCN sat down with retired WSNA Executive Director Dr. Sally Watkins. Watkins earned her BSN from the University of Texas System School of Nursing before moving to Utah to study for her master’s degree in nursing administration from the University of Utah College of Nursing. After two decades of working in nursing administrative roles, Watkins returned to school to earn her doctorate in philosophy from the Union Institute & University. A practicing RN for more than 45 years, Watkins served on the WCN board of directors from 2017-2021, helping to guide our work. As a nurse leader, Watkins “… consistently worked at building the power of nurses across Washington state to speak up for themselves and their patients in both the Legislature and the workplace.” –WSNA 2022 Hall of Fame Inductee
Here is what she had to share with us about her nursing journey.
WCN: What inspired you to pursue a career in nursing?
Watkins: It has been in my wheelhouse since I was little. My mom told me I wanted to be a nurse when I was three. I wanted to make a difference in people’s lives. In junior high, I lived in Dallas, TX, and volunteered at a hospital there through a volunteer program. It was more than delivering flowers and reading letters to patients. For a time, I was assigned to work in central supply. We learned how to fold towels, sheets, and gowns for the operating room before all the disposable supplies they have now. We had a nurse instructing us on how to do it correctly because there is a trick to doing it so the operating room team could open them up without contaminating anything. That fascinated me. I thought, wow, what would it be like to work in an operating room and to use the things we were putting together in these packs?
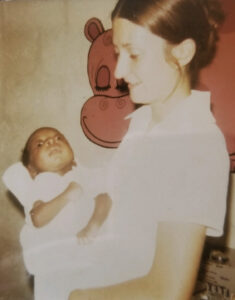
In college, between my sophomore and junior years, I decided to see if nursing was still what I wanted to do and applied to work as a missionary in Haiti for the summer. I went by myself, meeting up with other healthcare workers there. As a student, I worked for three months in that hospital, where they let me do a lot. It was a great experience. And challenging, too. I didn’t speak the language and had to learn some Creole and French to care for patients. Through that experience, I knew being a nurse was my calling.
WCN: Can you briefly share your journey into nursing leadership (career progression)?
Watkins: Directly out of nursing school, I thought I wanted to be a nurse midwife. Obstetrics has always been one of my areas of interest. I looked at several graduate programs across the U.S. and picked one in Salt Lake City. At the time, you had to work for a year before they would admit you into the program. You don’t see that requirement much anymore, but they had it then, so I moved to Salt Lake City to work and prepare to enter the program.
I was hired to work in the high-risk OB unit at the University of Utah Hospital. It included labor and delivery, postpartum, antepartum, and newborn nursery. I enjoyed working with high-risk patients, and I knew if I became a midwife, I would not be able to keep those women as patients. They would need a referral to a physician or a perinatologist. That created a dilemma for me.
Soon, I moved to Boise, ID, and worked in an OB unit at a hospital there. Since I had my BSN, they immediately put me into an assistant head nurse position. That was my first formal administration position in nursing. I learned a lot while managing that unit and had some great mentors helping me along the way. I returned to Salt Lake City to work in high-risk OB again. There, we had a transport system that would pick up high-risk OB patients. We covered something like seven states with both air and ground transport to bring these high-risk patients to the University Hospital. I worked clinically on the unit and the transport team for a while before being offered the head nurse position for the OB unit. In nursing, the more you do, the more you get to do.
I still wanted to return to school, and since I liked working with high-risk patients so much, I thought about becoming a clinical nurse specialist. I talked to a nurse executive I knew, and she said, “We have a hospital filled with nurses who are clinicians. But what we don’t have are nurses in formal leadership positions to lead those nurses.” She recommended I get into a nurse administration program. And that’s what I did. I finished my master’s at the University of Utah with a focus on nursing administration.
After about ten years, I was recruited to be the nurse administrator for Tacoma General Hospital here in Washington. It was more responsibility, but I felt I was ready for it. In Salt Lake, I had been responsible for units other than OB as other managers came and went. For example, if the person overseeing the psychiatric unit left, I would be responsible for both the OB and psychiatric units for a while. I also managed the burn unit for a time period. And even though I didn’t have the clinical expertise, what they needed was leadership knowledge, and that I had. So, I felt ready to take the position at Tacoma General. After ten years there, I was promoted to Vice President and Chief Nurse Executive for MultiCare. I did both jobs (administrator for Tacoma General and Chief Nurse Executive) for a while, then focused on the chief nurse position for the health system. At this time, I went back to school for my doctorate. I had finished my coursework, but there was no way I could finish my dissertation while working my job at MultiCare. The job required too much attention. So, I quit the job to finish my dissertation. While taking time off work, WSNA (Washington State Nurses Association) approached me about applying for the director of nursing practice, education, and research position. That was my first introduction to working for a state organization rather than in acute care.
Beyond working for a single hospital or health system, working for WSNA was an excellent opportunity to influence nursing practice across the state. I also got involved on a national level through the American Nurses Association. I found I really enjoyed focusing on different legislative issues, trying to increase the continuing education offered by WSNA, and gaining exposure to nurses across the state in terms of what their practice settings were like. After six or seven years, I wanted to get back into acute care to keep my pulse on issues nurses were facing, so I worked with CHI Franciscan for three years as an administrative director for clinical resource management. When I saw the WSNA Executive Director position posted, I was eager to apply. Going back to WSNA felt a lot like going back home. I felt fortunate when I got the job.
Additionally, while at WSNA, I taught a health policy class to DNP students at Pacific Lutheran University and became a pro-tem member of the Nursing Care Quality Assurance Commission.
Over the years, I have served in multiple roles in nursing.
WCN: How would you describe your leadership approach?
Watkins: My leadership approach is collaborative. I appreciate the need for nurses and others to have a voice and to share their experiences, including where they see gaps in our ability to provide quality patient care. I’m very open to listening to their concerns and feedback as well. So, I would say I’m a good listener.
One of the best compliments I have gotten was from the CEO at the hospital I worked at in Salt Lake. He said what he appreciated most about me was that I was calm and a voice of stability. When things aren’t going well, I don’t panic. I keep pushing forward, networking with those I need to get to a resolution. I’m not reactionary and avoid going off on tangents. I work to consider everybody’s point of view.
WCN: From your perspective, what attributes are important to be an effective nursing leader?
Watkins: To be an effective leader, you need to know yourself. You need to know your strengths and weaknesses. And where you are weak, you need to work on improving and ensuring you bring in team members with expertise in those areas. Nobody can do it all. Knowing where you need help and building a team reflective of different expertise and experience is important.
The other thing is organizational skills. Leaders should have the ability to manage their calendars the best they can. It is also imperative to be prepared and on time for meetings. If there are materials to read ahead of time, read them so you are ready for the discussion. Additionally, coming up with some questions you want answered and to get the dialogue going is helpful.
WCN: What do you enjoy most about the profession of nursing?
Watkins: Well, that’s easy. I believe nursing is the best profession ever. If I could start all over, I’d still pick nursing. A lot of it is because there is so much flexibility and opportunity. If you don’t like one area of nursing practice, choose something else. There are a lot of areas where nurses can have influence and use their power to effect change. The best thing about nursing is our ability to influence care delivery.
I’ve always been biased that nurses are trained to focus on the patient as a whole, not just the single diagnosis or complaint of the day. Nurses ask who the person is and about their support system. They ask where they live and what are the other issues impacting their health. It is not just a single diagnosis. During a conversation, you can discover another concern the patient might have. I think that is unique to nursing. That is another reason I would choose nursing again; we are very holistic in our view of the patients and the communities we serve.
WCN: You have seen a lot of changes in the nursing workforce throughout your career. What do you find encouraging? Where is there still work to do?
Watkins: In terms of improving care, we’ve made a lot of progress. But during COVID, we saw a lot of red flags on the playing field. We were not prepared as a country to take on a pandemic. It was embarrassing that we didn’t have what we needed. There is plenty of opportunity for improvement. I want to thank the nurses on the frontlines who spoke up and shared what was happening so we could be made aware of the issues they were facing. PPE was a big thing, but other issues still need to be addressed. Staffing is a big one. It’s not only acute care. It could be long-term care, community-based settings, home care, or school nurses–all of them need safe staffing systems in place.
The other area is growing our own. Nurses can lead from where they stand. There are nurse leaders in a variety of positions and roles. Some are in direct care. They are the charge nurses, the union reps, and the nurse managers. They are also the people who can move into those roles or into formal leadership positions. They can be in the C-suite or in organizations like WSNA, ANA, or WCN. Nurses can serve in all kinds of roles, and their leadership skills should be recognized and utilized to help make change where change is needed.
WCN: America’s healthcare systems are marred by structural racism and bureaucracies that contribute to health inequities. How do you see nursing contributing to action-based solutions to improve access to quality healthcare for everyone?
Watkins: One, we need to use our voices. Nursing is the largest health profession in the country, and we should work on unifying and using those voices. One thing I find irritating, especially when working with the legislative process, is nurses fussing with nurses. We can’t do that. Ultimately, we want the same thing–improved care for patients, communities, and families. We need to speak from that base. Using our unified voice to improve care is the biggest thing.
Second, I think it is the nurse leader’s job to help ensure environments where other nurses and healthcare practitioners work are healthy. Nurses can be successful when they have everything they need to provide quality care. Nurse leaders need to be willing to listen to and hear the bad news from their frontline staff to understand fully where to focus their attention.
The other thing is to be willing to compromise. You usually can’t get what you want right out of the gate. You need to know what you have to have first and what can come in second. I have learned that through the rules writing process or in legislation. It takes several different runs to try to improve things. You also must be collaborative while willing to compromise. You need to use your network of colleagues to ensure you are capturing the multiple perspectives correctly. You must know your priorities and where you will draw your line in the sand, but you also must be willing to bend a little.
WCN: What advice do you have for future nursing leaders?
Watkins: Be involved. And not just within your organization but in many ways. Be involved in professional organizations like WSNA, ANA, or WCN. And this is even more true if you want to affect legislative change. Also, be resilient. Don’t give up. As I mentioned earlier, if you don’t get everything you want on the first try, you have to be willing to come back again.
The other thing is having the willingness to develop other nurses. It doesn’t matter if they are a staff nurse, a nursing student, or even a high school student interested in nursing; make sure you work to give them the information and experiences they might need to help them succeed.
While working on my dissertation, I interviewed nine nurses in CEO positions at large hospitals or health systems. I asked them a similar question. They gave me a list I thought was great: 1. Be yourself. Know what your priorities are and what you want to do; 2. Honor relationships, find good mentors, and focus on the big picture; 3. Take advantage of every opportunity. If a project needs to be done, step up and do it. The experience will help you to grow; 4. Be willing to work hard; 5. Become a good communicator; 6. Your actions must be consistent with your values. If you really care about patients, your actions should speak to caring about patients; 7. Continue to learn and to want to learn; and 8. Implement succession planning.
This list offers excellent guidance for any future nurse leader.
WCN: Is there anything else you want to share with our audience?
Watkins: As someone with a nursing administrative background who went to work for WSNA, it was interesting to me that WSNA wasn’t considered a professional nurses’ association but was seen by some as “just” a Union. However, I think of WSNA as a professional organization for all nurses in Washington state. Some nurse administrators have had issues working with the Union. But as someone who has represented both sides of the table, I have always believed that nurses really work with nurse leaders, and, as I mentioned earlier, those nurse leaders are responsible for the working conditions of nurses. To me, there was never a conflict. Nurses with the potential to become future nurse leaders can come from those nurses who take on representative roles in the Union, such as union reps. It is a great way for a nurse to learn new leadership skills and the responsibility of communicating at different levels with different concerns.
Some nurse leaders see this chasm between those in leadership roles and those on the frontlines. I think that is sad. That is where I think we need to do more work on unifying our voices because, ultimately, we want the same thing for our patients and the communities we serve.

