

An interview with Victoria Fletcher, RN, MSN, ARNP, FACNM
A renowned nurse leader, Fletcher is a certified nurse-midwife and fierce advocate for nursing workforce diversity. Fletcher earned a BSN from the UW School of Nursing in 1973 and an MS in Nursing from the University of Illinois, Chicago, in 1978. Fletcher spent her career as a tireless champion for health equity and the elimination of health disparities in communities of color. A mentor for all nurse leaders, Fletcher served 17 years on WCN’s Board of Directors, and her contributions and service to nursing are extensive.
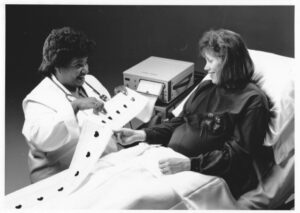
Victoria Fletcher, RN, MSN, ARNP, FACNM retired from Planned Parenthood Federation of America, where she served as Senior Analyst and Lead Surveyor in the Accreditation & Evaluation Department and was previously Director of the Affiliate Operations Evaluation, Accreditation and Evaluation Department. After retiring from her administrative position at Planned Parenthood, she continued working part-time as an Advanced Practice Clinician at Planned Parenthood of the Great Northwest and the Hawaiian Islands. Her experience includes healthcare administrative roles, providing direct patient care as a nurse-midwife, and, as a nurse educator, providing didactic and clinical experiences to undergraduate and graduate nursing students, including nurse-midwifery students.
She has long worked to advance nursing practice and leadership in nursing. She has served as chair of the Washington State Nursing Care Quality Assurance Commission (formerly Washington State Board of Nursing) and later served as a pro tem member. She has been actively involved with several community and professional organizations, including the Washington Health Benefit Exchange Advisory Committee, the Ebony Nurses Association of Tacoma, the Washington State Department of Health’s Health Innovation Leadership Network Communities and Equity Accelerator Committee, the American College of Nurse-Midwives (ACNM), Association of Women’s Health, Obstetric and Neonatal Nurses, Health Coalition for Communities of Color, WithinReach, March of Dimes, the Washington Association of Black Professionals in Healthcare and the ACNM Midwives of Color Committee. Mentoring aspiring nurses and other healthcare professionals has been a consistent theme throughout her career and community service. Accolades include the Distinguished Diversity Advocate Award from the University of Washington School of Nursing, the Miriam Manisoff Advanced Practice Clinician Award from the Planned Parenthood Federation of America, and the ACNM Foundation Clinical Star Award for over 25 years of excellence in clinical practice and mentoring nurse-midwives.
Here is what she had to share with us about her nursing journey.
WCN: What inspired you to pursue a career in nursing?
Fletcher: I grew up in Detroit, MI, during the 50s and 60s, when they still had segregated hospitals. I frequently went with my mom to visit relatives or acquaintances in the hospital and had the opportunity to go to both the segregated and desegregated hospitals. Even from a child’s perspective, I noticed the differences. The resources were much less at the segregated hospitals. It even looked dimmer and barer than the other hospitals. I wondered why there were differences. These experiences inspired me to be in a helping profession, to make sure the quality of care available to people of color was the same as it was for anyone else. My uncle, Dr. Howard Venable, a renowned Ophthalmologist, also encouraged me to go into a medical-related field, either medicine or nursing, and I ultimately chose nursing.
WCN: Can you share your journey into nursing leadership (career progression)?
Fletcher: I graduated from the University of Washington (UW) and started working on a med-surg unit. I worked there for a couple of years, which was good as it provided me with a wide variety of patients and experiences. I then decided I wanted to venture into the obstetrical field. Bedside nursing was great, but the appeal of becoming an advanced practice nurse (a relatively new role at that time) was intriguing. I thought, how can I combine obstetrics with advanced practice nursing? During my undergraduate program at UW, one of my professors and mentors was a nurse-midwife, and she shared with me why she chose Nurse-Midwifery as a profession and the education requirements. From her encouragement, I decided I wanted to become a nurse-midwife!
I encountered obstacles because nurse-midwifery programs did not want to accept students who did not have prior obstetrical experience. However, I did not let that deter me. I kept applying to different programs and was eventually accepted for admission by the University of Illinois Chicago.
The nurse-midwifery role added new dimensions to my nursing role. It included leading and directing the management of the patient’s care, and in terms of perspective and skills, I found that very fulfilling.
My husband was in the Navy, and if we moved to a locale without a nurse-midwifery program, I would seek work as a nursing educator. I have taught nursing in California, South Carolina, and Washington State, allowing me to mentor students and advocate for increased diversity in the nursing workforce.
When I graduated, I had a substantial amount of student loan debt. To help pay back the loans, I joined the National Health Service Corps. To qualify for the program, you agreed to work for three years in an underserved area, and in return, they would pay back approximately 85% of your student loans. That would be a tremendous financial help, so off we went to South Carolina, and I worked with the National Health Service Corps at a Federally Qualified Health Center in a low-resourced area. I had patients who could not read and write, who did not have running water, and many lived below the poverty line. Health equity was not terminology in vogue back then, but I knew all people deserved quality health care and the best of whatever was out there. I tackled my practice there in the same way. I practiced nurse-midwifery and was affiliated with the Medical University of South Carolina where the patients delivered.
I left the Corps, and the Medical University of South Carolina invited me to become full-time faculty. Being a faculty member, I was able to influence many students and hopefully help them on their journeys to deliver quality care to all.
While working as a nurse-midwife, I realized that to impact and affect policies that lead to health inequities, I needed to bring my voice to the tables where the decisions were being made. That was the next step I wanted to add to my nursing career. It was not because I wanted to get away from bedside care. One of the things I am most proud of throughout my career is whether I was working in health administration, education, or health policy, I maintained a clinical practice. I negotiated that with my employers because I gained satisfaction and energy from clinical clients and clinical work. Plus, I needed my clinical practice to stay relevant and to know what was happening on the front lines.
I also did other things when I had the opportunity. You must take a chance on yourself and act on opportunities. You do not have to be in it by yourself. You can look for mentors. That is how I got involved with the March of Dimes, and later, an organization called WithinReach (then called Healthy Mothers Healthy Babies). A mentor, the late Cynthia Shurtleff, invited me to participate on the Healthy Mothers, Healthy Babies board, where I served for 20 years. WithinReach uses an interdisciplinary approach to build pathways to make it easier for Washington families to navigate complex health and social service systems and connect with the resources they need to be healthy and safe. There were people on the board from business, health care administration, and health plans, which I found helpful. I got to see how thought leaders from different sectors think about healthcare. And from there, I learned about opportunities to serve on the State Board of Nursing. I applied and was appointed by Governor Booth Gardner and reappointed by Governor Gary Locke. There, I knew I would have the opportunity to impact and influence nursing practice.
During my time at the Commission, a coalition of nursing leaders, labor unions, nurse educators, and nursing organizations convened a summit to explore creating a nursing workforce center. We were in the grasp of the nursing shortage and did not have much data or information about the nursing workforce in Washington. We needed the nursing workforce center to support the Nursing Commission, employers, educators, and policymakers in making evidence-based recommendations to address the shortage. The Washington Center for Nursing (WCN) was established as a result of this process and legislative action. I was not on the initial WCN board but was elected about two years after its inception… I wanted to serve on the board because, despite all the things I and others were doing, I did not see a lot of ethnic and racial diversity in the nursing workforce. Again, back to what I had noticed as a child, health outcomes were worse for communities and people of color. On the WCN board, I could help influence and advocate for increased diversity in the nursing workforce. It was another aspect of advancing my desire for all people to receive quality health care that would result in good health outcomes.
I never shied away from taking on distinct roles. That is something appealing about the nursing profession. Many times, nurses put themselves into a box and may not seek the wide range of opportunities that are out there. Nursing prepares people to think critically, use good judgment, perform highly skilled tasks, conduct research, and implement evidence-based practice. Those skills are in high demand and are transferable to a wide range of job and career opportunities. It is valuable for nurses to look at opportunities to apply their nursing knowledge and skills to other areas. That is where you will encounter a broad array of thought leaders, influencers, and policymakers. There may be a learning curve, but nurses can exert much influence when they utilize their considerable knowledge, skills, and abilities in the broadest sense. I cannot think of an industry or sector that would not benefit from having a nurse at the table.
WCN: How would you describe your leadership approach?
Fletcher: I try to create a collaborative approach and an environment of healthy descent. I am not the type of leader who must have everybody around me agreeing with me or rubber-stamping whatever I say. When people feel safe challenging something and speaking their minds, they make better decisions. I want to encourage practical solutions that will work for people. When people are not afraid to speak truth to power, there is a better chance of creating impactful solutions. I also like to surround myself with people with different skills than I have so we avoid a group-think situation. The most successful teams I have collaborated with had people with different but complementary skill sets.
I have also learned to ask if there is more than one way to accomplish the goal/task and try to impart this idea when teaching or mentoring nurses. It is important to understand that there are multiple ways to do certain things. But you need to know the difference between those things where you absolutely must do A, then B, then C, and then D from things where you might be able to do A, then D, and then come back and do B and C. It causes concern when somebody tells me the reason to do something a certain way is because that is how it has always been done. Being too rigid can limit innovation. We all need a little MacGyver in today’s fast-paced and rapidly changing environments.
In terms of leadership, you must be prepared to lead. If you get a briefing book or documents ahead of a meeting, you need to review them and come prepared to participate. From my time at the Nursing Commission, where we had to read thousands of pages in preparation for meetings/hearings, and I am not exaggerating, I practiced delineating the essential information that would aid me in being prepared with at least one question, inquiry, or comment related to each agenda item. It will help you gain insight, contribute, and be a valuable member of the team.
Additionally, to be an effective leader–you must be resilient!
WCN: What do you enjoy most about the profession of nursing?
Fletcher: I enjoy how multifaceted nursing is. You can do almost anything if you are prepared as a nurse. In one of my leadership positions, we recruited a nurse clinician/practitioner with a background in informatics because we were designing templates for use in an electronic health record (EHR) system that all providers, including nurses and nurse practitioners, would be using. Typically, an IT person would design it. That was also the plan at the organization where I worked. I said, no, we should have a nurse lead or co-lead the project and implementation. Nurses with IT backgrounds do exist. I was the first in the affiliated organizations to bring a nurse to the project, and we had a much better implementation, rollout, and user satisfaction than other affiliates that did not have a nurse in this critical role. It worked better because the end users, nurses and nurse practitioners, were included in the design. At the affiliates without an informatics nurse on the design team, from the IT perspective, the EHR worked, but it did not work well for end users and did not fit into the workflow of the clinical sites.
The other thing I enjoy most is encouraging young people to get excited about a career in nursing. One step I took was setting up a scholarship at my alma mater. It is an endowment that offers scholarships to racially and ethnically diverse students who want to pursue nurse-midwifery or women’s health. The scholarships can be used for expenses beyond tuition. The funds may be used for wraparound services like transportation or childcare if that will contribute to the student’s success in the program. Everyday people coming together to contribute small amounts of money, when taken together, can create something meaningful. I encourage everyone to look at ways they can help lend a hand to support the next generation of nurses.
WCN: You have seen many changes in the nursing workforce throughout your career. What do you find encouraging? Where is there still work to do?
Fletcher: It is encouraging that, year after year, nursing is voted the most trusted profession. It is wonderful that the public holds nurses in high regard. Wages and benefits are better at recognizing nurses as highly skilled professionals who should be compensated accordingly, but they are not yet where they need to be. For instance, we are still pursuing pay equity for advanced practice nurses. Compensation should be the same for the same service, whether performed by a physician or advanced practice nurse. We have made strides, but there is still more work to do.
My personal objective continues to be to increase the ethnic and racial diversity of the nursing and healthcare workforce. Any projects I spend time on now involve advocating to meet this objective. There have been so many studies that show that culturally congruent care improves health outcomes, and I want this care to be readily available in our communities. In the spotlight currently is the issue of maternal mortality. Maternal mortality for African American women in the U.S. is four or five times higher than for the Caucasian population. Too many women are dying. It is estimated that three-fourths of these deaths are preventable, which is incredibly sad. The problem is not only related to social-economic or insurance status or education level. We have all heard the stories of several high-profile celebrities who experienced preventable complications and even death during or after childbirth. All women, but especially all African American women, are at risk. There is much to do on this front right here in the United States.
WCN: America’s healthcare systems are marred by structural racism and bureaucracies contributing to health inequities. How do you see nursing contributing to action-based solutions to improve access to quality health care for everyone?
Fletcher: I think we can go a long way by acknowledging that racism and inequities exist. It is detrimental to healthcare when it is said that structural racism does not exist. Saying it exists is not saying a person is bad. Though sometimes that is what people hear. Structural racism is hard-wired into the system, and we must acknowledge it. It does not help to bury your head in the sand and say it does not exist. The recent work at a Seattle hospital, where they had an external entity come in and assess their entire institution, including policies, produced results that cannot be ignored or denied. The consultant called out examples of structural racism, policies that disproportionately impacted patients and families of color, and the stark lack of ethnic and racial diversity in the hospital’s staff and management. Given this critical information, the hospital has now recommitted itself to eliminating the vestiges of structural racism and health inequities. It all starts with acknowledging that structural racism exists and then taking action to mitigate and eliminate the racist structures, policies, and practices.
Nurses must intentionally choose to be an ally in this work. I make the analogy to that of a bully. There is the person who does the bullying, and then you have the victim of the bullying. But frequently, you also have bystanders who witness the bullying but fail to act. I call these bully enablers. That is what we often have in nursing and healthcare in general. You may not be the fiercest anti-racism advocate, but if you want to be an ally, if you see something, say and do something. If you are in a room where decisions are being made and observe that the people who those decisions impact are not at the table, say and do something. Agreeing in principle that diversity and anti-racism efforts are admirable, lacks intentional action to change the status quo. Nurses can contribute by being what I call “activist” allies. It should come naturally for nurses because we advocate for our patients every day, and we must take it to the next level by dismantling unjust systems and eliminating bias in policies and practices.
I also think nursing education programs must do more to attract, admit, retain, graduate, and have successfully pass the NCLEX exams more racially and ethnically diverse students. Potential nursing students and their families deserve to know how successful nursing education programs are in graduating students who look like themselves. Nursing programs should adopt a common set of metrics that measure the performance of key diversity indicators that would be published and widely available to all stakeholders, including potential students. This level of transparency would help hold the programs accountable to the communities they serve. The data would aid in fulfilling the program’s obligations to their communities and potential students in those communities. Some nursing programs are in remarkably diverse neighborhoods and communities, yet their student population does not reflect that diversity. That is a problem. Educational institutions must use metrics and standards that allow them to be more inclusive and successful at educating diverse students. The Washington State Board of Nursing, educators, industry, employers, and businesses must work together to graduate a more resilient and diverse nursing workforce. WCN can help by building coalitions of people to work toward achieving common goals. A change in thinking reflective of the idea that students are the consumers of education programs, and, therefore, should have, at their disposal, all key information to make informed decisions about programs before they apply for admission. For example, it was uncomfortable when quality and performance measures were first introduced in healthcare, and now they are widely accepted and available. Consumers can access this data and make informed decisions about comparing providers, insurance plans, hospitals, etc. For example, you can find out the total hip complication rates at different hospitals in a geographic area. This data assists the consumer in deciding which hospital to select for their surgery. Nursing education is expensive and time-consuming. Potential students should see their value reflected in the education program’s curriculum, policies, and procedures. Admission, retention, and graduation rates, along with NCLEX pass rates for all students disaggregated by race and ethnicity, must be available to guide decision-making and to hold programs accountable. We must all do a better job.
WCN: What advice do you have for future nursing leaders?
Fletcher: Develop a mechanism to stay in contact with nurses and nursing-related issues on the front lines. Regardless of what arena you work in, you must have a way to interact with nurses and the critical issues they face at all levels. The worst thing is when a leader or policymaker has no idea of how regulations, policies, and procedures impact the people doing the work. Staying connected helps a leader stay relevant and helps to ensure that the policies and the work have a beneficial rather than harmful impact on nurses.
Nursing is a dynamic profession, and the individual nurse drives their own career trajectory. Nursing is a flexible profession that will take you wherever you want to go. Nursing knowledge, skills, and abilities are needed everywhere. Seek opportunities in traditional and non-traditional arenas. You are the only one who can make it happen, so take the steps and go for it!

